Dry eye syndrome affects about 20-30 million people in the United States. It is particularly common here in the often dry and windy Central Coast. The eye surface is a mucous membrane tissue much like the inside of our mouth. As such, the eye needs to stay moist in order for it to feel comfortable and so that we can see clearly. The loss of moisture from the eye surface often leads to a dry, scratchy, burning, gritty, tired or fatigued feeling. Sometimes the eyes may become watery because when the eye surface becomes dry, the tear glands release excessive “reflex” tears to wash over the eye. In many cases, patients may not even know their eyes are dry or feel any discomfort and may just have periods of blurred vision that comes and goes. The eye surface needs a smooth layer of tears covering it in order for an image to be clearly focused in the eye.
How do you know that you have dry eyes? Usually, the above symptoms alone are sufficient to make the diagnosis. You may also test your self by blinking a few times and then stare straight ahead with your eyes open and try not to blink. Normal eyes should be able to stay open for at least 10 seconds without vision blurring and without feeling aware that the eye is open or uncomfortable. If your test is less than 10 seconds then your eyes are probably dry. Your eye doctor may also look at the surface of your eye or use special tear dyes to see if the surface is dry or irregular. Your doctor can also test your tear production by placing small strips of filter paper on the edge of the eyelid for several minutes to see how much tears absorb onto the paper (Schirmer’s test).
Causes of Dry Eye
Most dry eye patients suffer from less production of tears that are common with aging. This is often made worse by tear evaporation in a dry, low-humidity environment. Once the eye surface becomes dry, the constant blinking of the eyelids over this dry surface begins to cause inflammation of the front of the eye. This can create a vicious cycle as the inflammation causes more damage to the tear glands, which causes fewer tears to be made, and so on. Sometimes the tear glands dry up from other conditions such as:
Decreased hormone levels (especially post-menopausal women).
Autoimmune diseases such as Sjogren’s syndrome, rheumatoid arthritis, lupus, etc.
Medications such as systemic antihistamines (most allergy pills), antispasmodics (bladder control or bowel spasm pills), and some Parkinson medications. Eye injuries (especially prior chemical splash to the eye) or eye surgeries (especially LASIK surgery).
Blockage of oil release from eyelid glands, seen in common conditions such as blepharitis (crusting and sometimes infection along the edge of the eyelids) or rosacea dermatitis (“adult acne” with clogged glands in the eyelid and often throughout the face).
Poorly functioning eyelids that do not hold in the tears very well. This is often seen in older patients who have loose eyelids that “sag and droop” or that turn in (entropion) or turn out (ectropion).
Visual tasks. Although using the eyes excessively will not cause harm to the eyes, it may cause eye fatigue and this is more common in patients with dry eye. When focusing with the eyes (especially reading or using the computer) the eyes do not blink as frequently and thus the tears can evaporate easier.
Treatment of Dry Eye
The goal of all dry eye treatment is to make the eye surface moister. This can be attempted in many ways. For patients with only mild dry eye, usually moisturizing regularly with artificial tears is sufficient.
1. Treat any underlying causes if they are present.
a.) Post-menopausal women may want to consider hormone replacement therapy.
b.) Ask your primary care physician about checking for and treating any autoimmune diseases.
c.) Consider changing any medications that have antihistamine or anticholinergic side effects.
d.) If you have eyelid gland clogging such as from blepharitis or rosacea dermatitis then daily eyelid washes with warm water to gently scrub away any crusting and open up the glands will be helpful. In addition, warm compresses applied to the eyelids several times a day will help to drain the glands easier. For patients with rosacea dermatitis, a course of tetracycline or similar pills will often help the glands of the face and the eyelids produce better oils that do not clog the gland pores.
e.) If you have been diagnosed with loose eyelids or in-turning or out-turning of the eyelid, talk to your doctor about an eyelid tightening surgery.
f.) If you smoke, stopping smoking will greatly improve your dry eye condition.
2. Use artificial tear replacements. All can be purchased over-the-counter without a prescription.
a.) Any brand is okay to use as long as it feels comfortable for your eyes. However, in general, it is best to use “preservative-free” tears. Preservatives are chemicals that allow the tears to be sold in a larger bottle but the chemicals can cause further irritation of your already sensitive eyes. Also, it is best to avoid those brands that advertise, “get the red out” (such as Visine or Murine) because, again, chemicals are added that may further irritate the eye surface.
b.) Brands that patients frequently report good success with include Refresh or Refresh Endura, Celluvisc, Systane, Bion Tears, Genteal, HypoTears, Moisture Eyes, and TheraTears. The new Nature’s Tears EyeMist spray helps some patients. A tear that is thicker stays on the eye longer and moisturizes better. However, the thicker tears may also blur your vision for some time after using them.
c.) Many patients like to use a tear ointment (such as lacrilube, Refresh PM, Duratears, etc.) before bedtime. This will moisturize all night and the thick ointment can be wiped away in the morning.
d.) Much like watering your houseplants, you should use artificial tears on a regular schedule (usually several times a day at least) and not wait until your eyes show signs of dryness before you moisturize them.
3. Your doctor may occasionally prescribe a topical anti-inflammatory medication.
a.) Restasis (ophthalmic cyclosporine) is a potent anti-inflammatory medication. By reducing eye surface inflammation it allows your own tear glands to heal and begin producing more tears. It is typically applied 2 times a day like and it may take several months to have its best effect.
b.) Some patients may be prescribed topical steroid drops for a short time.
4. Other treatments.
a.) Vitamin and dietary supplements. Pills containing omega-3 fatty acids, fish oil, flaxseed oil, and gamma-linolenic acid (GLA) have been shown to increase tear production. These are available over-the-counter with no prescription needed.
b.) Moisture-chamber glasses. Trapping moisture around the eyes may help patients with severe dry eye. Swimming goggles worn at night may help, or many companies sell eye goggles such as Panoptx eyewear available at the www.panoptxpro.com website.
c.) Punctal occlusion. Your doctor may recommend that the small drain hole of the upper or lower eyelid be closed with a very small punctum plug. This is a painless office procedure that only takes a few minutes. By decreasing the drainage of tears out of the eye, the small number of tears that your eye makes can keep your eyes moister. The plugs are usually made from silicone and can be removed if requested. Rarely the punctual drain can be permanently closed with surgery if needed.
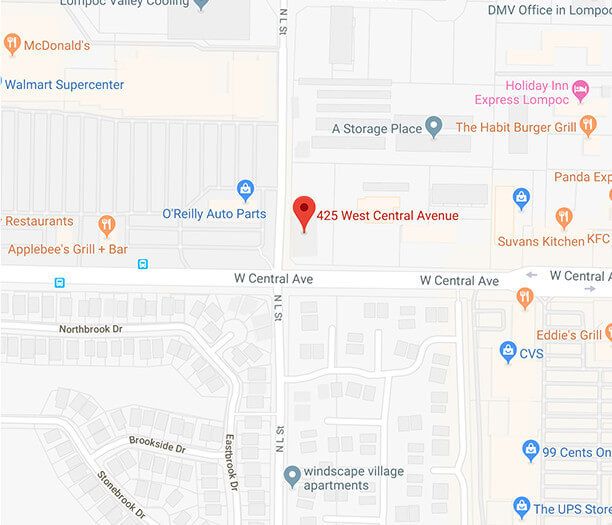
For further information or to schedule an eye exam please call our office at (805) 925-2637 in Santa Maria or (805) 736-2020 in Lompoc.